
Treatment
Musculoskeletal medicine is a medical discipline that deals with pain and disordered function of the muscles, joints, tendons, ligaments, nerves and associated tissues.

Mobilisation and Manipulation
Musculoskeletal practitioners may use mobilisation or manipulation to help with pain and improved range of movement.
Read More
Prolotherapy
Prolotherapy is a safe, effective injection treatment which provides increased strength in joints, ligaments and tendons by making new connective tissue.
Read More
Exercises
Exercise keeps cartilage, bone, and muscles strong by continually remodeling and building structure.
Read More
Perineural Injection Therapy
In Neural Prolotherapy, the subcutaneous (under the skin) nerves are recognised as a source of pathology.
Read More
Cognitive Behavioural Therapy (CBT)
CBT is a method of pain management used by many musculoskeletal medicine practitioners.
Read More
Trigger Points
A trigger point is a portion of the muscle that has become a source of pain and spasm.
Read More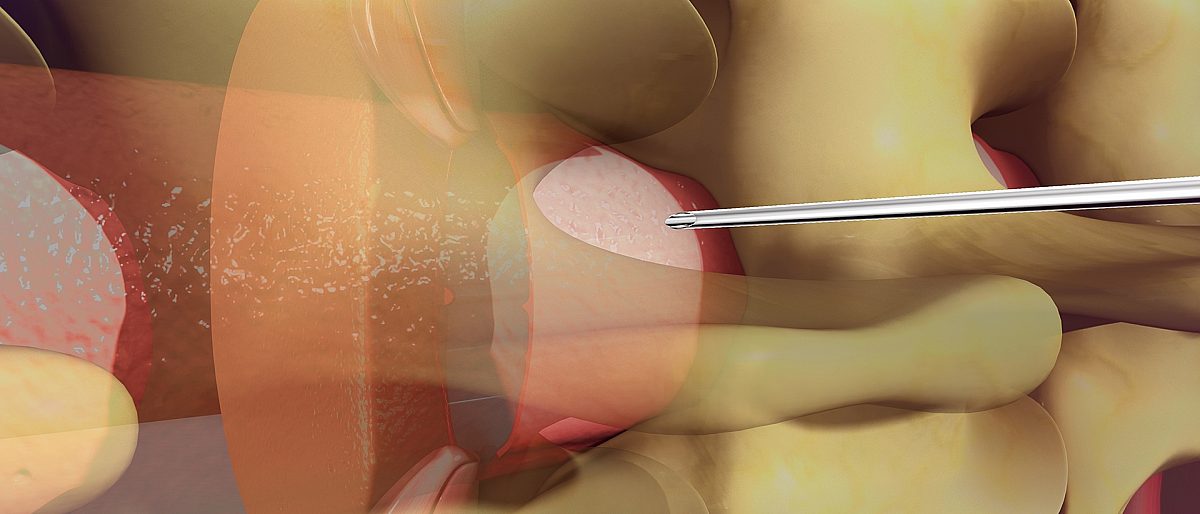

Joint injections
Joint injections can be an effective way of treating some disorders of joints and ligaments that are caused by inflammation such as osteoarthritis, inflammatory arthritis (eg: gout), and shoulder or hip bursitis.
Read More
Neural Therapy
Neural therapy is a German technique involving the injection of local anesthetics into scars, based on the theory that scars can produce long-standing pain and malfunction.
Read More
Nerve Blocks
When discs or osteoarthritic facet joints press on a spinal nerve as it emerges from the spine, the nerve is irritated and swells up causing severe pain that is usually felt down the buttock or leg (sciatica).
Read More
Acupuncture
For more detail on acupuncture see the website of the Australian Acupuncture and Chinese Medicine Association
Website